A Comparison of Methods of Producing a Discharge Summary: handwritten vs. electronic documentation
Claire Pocklington and Loay Al-Dhahir
Cite this article as: BJMP 2011;4(3):a432
|
|
Abstract Background: It is a compulsory requirement that a hospital produces a discharge summary. This is often the only documentation a GP receives in relation to a recent admission. Traditionally the discharge summary is hand-written and commonly known as the TTA (‘to take away’). Recently the EDS (electronic discharge summary) has been introduced. This audit provides a comparison of the TTA and EDS. Methods: A random sample of 50 TTAs and 50 EDSs were selected from one ward over a two-month period. Completion rates for criteria of the discharge summary were analysed. Results: The EDS is a superior form of discharge summary, significantly for documenting diagnosis, co-morbidities, investigations, drug history and instructions for the GP. Conclusions:Junior doctors should be more aware of the importance of the discharge summary; therefore they should provide clear, complete and concise information. In order to ensure EDSs are completed correctly training on using the computer programme should be more thorough. Documenting co-morbidities has implications on clinical coding. Other healthcare professionals should contribute to the discharge summary. Keywords: discharge summary, TTA, EDS, handover, information |
Introduction:
On discharge from hospital, secondary care providers have a duty and obligation to communicate with primary care provides – particularly the general practitioner – to give information regarding the reasons for admission, results of investigations, procedures performed, treatment instigated and importantly follow-up management. Therefore the transition of information between secondary and primary care is vital for care management and hence patients’ safety.
This information is shared in the form of a ‘discharge summary’. It is the responsibility of the secondary care team to provide this. The level of detail given has been found to vary not just between different NHS trusts or hospital but also between different wards and individual doctors completing the discharge summary – this can create many problems as communication plays a pivotal role in patient care.
The information given in the discharge summary is all that a patients’ GP knows in regards to their hospital admission and management. A discharge summary is effectively a form of ‘handover’. A hospital physician may instruct the GP to do certain things in regards to follow-up; for example check blood results, review results of investigations arranged as outpatients or simply review the patient clinically. The more information that is transferred across from secondary to primary care the more awareness the GP has to what has happened and what needs to happen, which leads to better patient care.
A discharge summary can also be a valuable document for when a patient is admitted to hospital; if their notes are not available a past discharge summary will provide useful information (re. past medical history and drug history in particular) to the medical team who may have no prior knowledge of the patient, this is invaluable if it not possible to take a history from a patient and is also useful in directing investigations if a patient has been admitted with the same complaint(s). Of course this depends on the patient having a copy of the discharge summary with them on admission or the ability to access previous discharge summaries electronically.
Good documentation is vital in the healthcare setting. All documentation, no matter in what form, must be clear, accurate and legible. Any type of document is useless if it cannot be read. The GMC and Royal College of Physicians stress the importance of documentation1, 2.
The importance of the discharge summary has been highlighted in the last few years. There has been a move from the traditional hand-written discharge summary – commonly referred to as the TTA (to take away) – to the use of computer software providing an electronic discharge summary (EDS). The latter not only provides more detail but also aims to deliver it to the primary care setting in a timelier manner; for example, in the future, once all EDSs are completed at Barking, Havering and Redbridge University Hospitals NHS Trust there are plans for them to be automatically emailed to a patients GP surgery – currently this scheme is being trailed at certain GP surgeries. This complies with the requirement and recommendations made to secondary care trusts to provide the GP with a discharge summary within 24hrs of a patients’ discharge from hospital – consequently reducing previous financial penalties when not achieved and thus being more cost efficient.
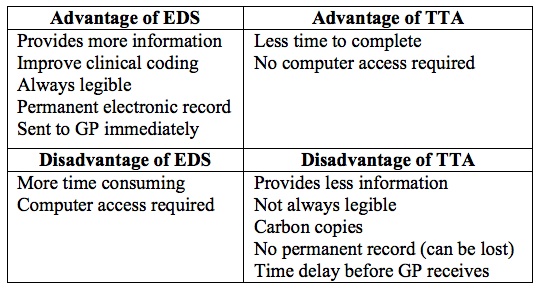
The advent of the EDS has impacted the daily working of the junior doctor, who is commonly, the individual on the secondary care team whose role it is produce the discharge summary. Previously with a TTA a patient could be discharged home without all the constituents on the form being completed and so a GP would be provided with an incomplete discharge summary. At BHR University Hospital NHS Trust in order to produce a finished EDS - and essentially discharge the patient - all constituent sections have to be completed before it can be electronically sent to pharmacy so that the patient sent home with their medications (the discharge summary acts as a prescription). Therefore producing an EDS is more time consuming in comparison to a TTA. However an EDS does have advantages (see Table 1).
Table 1: Comparison of EDS and TTA
Any form of discharge summary is user dependent; what is written is determined by the individual doctor producing the document therefore there is no guarantee that they have documented everything that occurred during admission. In the case of the TTA user dependence also refers to the legibility of the writing, the durability of the carbon copies produced, as well as the level of detail of the discharge summary produced.
In 2008 Newham University Hospital Trust introduced the EDS, the trust audited this process and found it to be successful3. 2010 saw the introduction of the EDS at BHR University Hospital NHS Trust. The EDS was piloted on Sunrise B ward of Queen’s Hospital, Romford. The purpose of this audit is to establish if the introduction of the EDS at BHR University Hospital NHS Trust has been successful. The audit aims to determine if the EDS method is superior to that of the traditional TTA – this will be achieved by comparing the completion rates for specific criteria of the discharge summary. This audit also aims to identify areas of improvement and recommendation for the EDS.
Design and Method:
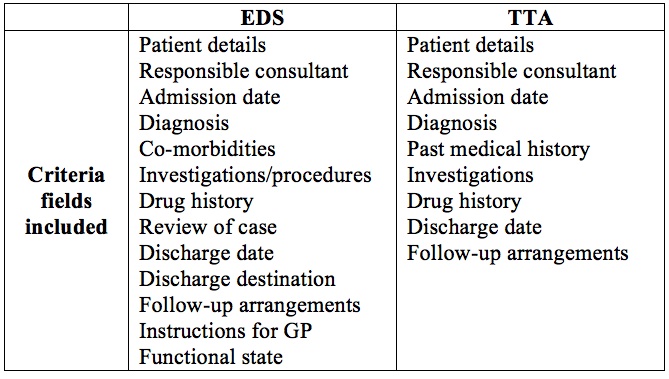
An opportunistic sample of 50 TTAs and 50 EDSs were selected from the patients admitted to Sunrise B (‘Care of the elderly’) ward, Queen’s Hospital, Romford in a two-month period (January to February 2011). Thus this is a retrospective audit. No exclusion criteria for selection of discharge summaries was set. For each discharge summary completion rates for the different fields of the discharge summary were recorded. Table 2 shows the criteria fields included in each type of discharge summary.
Table 2: Comparison of EDS and TTA criteria
The Royal College of Physicians have published their recommendations for the structure and content of the discharge summary. Section headings include
- GP details - name, address, practice code
- Patient details – surname, forename, date of birth, gender, NHS number, address, telephone number
- Admission details – method of admission, source of admission, hospital site, trust, date of, time of
- Discharge details – date of, time of, discharge destination, discharging consultant, specialty
- Clinical information – diagnosis at discharge, operations/procedures, reason for admission/presenting complaint, allergies, investigations and results, treatments, discharge medications, medication changes
- Advice, recommendations and future plan – hospital/GP/community
- Person completing summary – doctors name, grade, specialty, signature, date of completion4
This audit establishes which method of discharge summary is more compliant with these recommendations.
Data analysis was mainly descriptive. Data collected was tabulated and represented as percentages. Graphical representation of the data was performed using Microsoft Excel. Due to the nature of the study and data collected more sophisticated statistical analysis, such as that requiring the use of SPSS software, was not warranted.
Results:
Results demonstrate significant differences between the TTA and EDS completion rates for criteria of the discharge summary. Table 2 presents the data as percentages in a tabulated form. Compared to the TTA, the EDS had a higher rate of the following six criteria of the discharge summary documented; diagnosis, co-morbidities, investigations, drug history, discharge destination and instructions for GP.
Table 3: Summary table of data
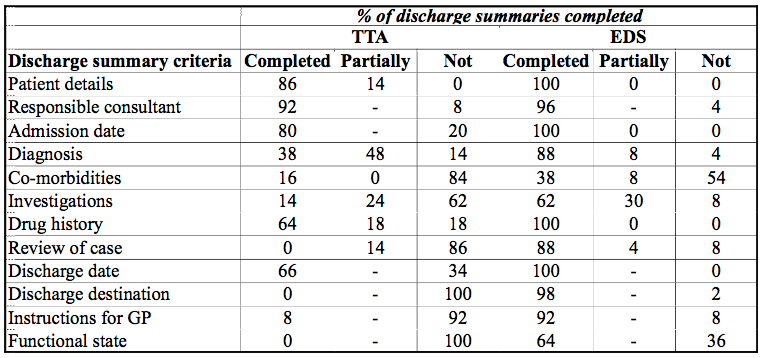
- Patient details and admission date.
The TTA had lower completion rates for these fields than the EDS. The EDS software automatically enters these fields therefore it is not possible for this criterion to be incomplete. The correct patient details ensure continuity of care and patient safety. If patient details – i.e. full name, date of birth, hospital number and address - are not present those with similar names could be mixed up.
Diagnosis.
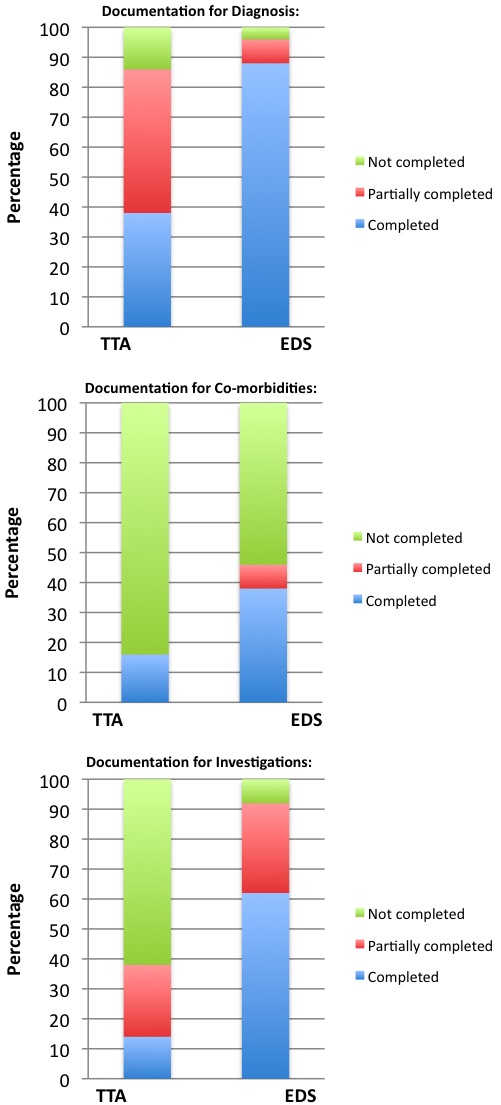
The TTA performed poorly on documenting diagnosis. The EDS had a completion rate significantly higher than that of the TTA (EDS completion rate = 88%, TTA completion rate = 48%). Figure 1 represents these findings. The main objective of a discharge summary is to inform primary care of the diagnosis to enable healthcare management, therefore it is crucial and pivotal information, for it not to be included in the discharge summary is illogical.
Co-morbidities.
Neither TTAs nor EDSs documented co-morbidities well. However the EDS, yet again, outperformed the TTA. See Figure 1. Documenting co-morbidities has important repercussions for clinical coding and financial incentives (see below).
Investigations.
Coincidently, 62% of TTAs did not document investigations that the patient had had in contrast to 62% of EDSs that did. See Figure 1. There is no guarantee for either discharge method that all investigations are listed; it is dependent upon the doctor who is producing the discharge summary.
Figure 1: Graphical representation of data
Drug history.
As previously mentioned, EDS has to have a completed drug history before the patient can be discharged and hence they have to have a 100% completion rate for this criterion. TTAs only achieved a 64% completion rate as Table 3 demonstrates.
Review of case.
This is not a criteria field on the TTA document. Therefore 86% of TTAs provided no review. 88% of EDSs did provide a case review. Just fewer than 10% of EDSs were incomplete for this item.
Discharge date.
Like the admission date, a discharge date is automatically completed on an EDS thus the completion rate is 100%. However, this date is the date in which the EDS is completed and may not be the actual day the patient leaves hospital because sometimes the EDS is completed (and so the medications dispensed) the day prior to discharge or patient discharge may be delayed. The TTA achieved a 66% completion rate.
Discharge destination.
This is not a criterion present on the TTA and thus 100% of TTAs did not fulfil this requirement. EDSs had a 98% completion rate.
Follow-up arrangements.
The majority of EDSs documented the follow-up plans for a patient (88% in total, 70% specifically for GP follow-up). 46% of TTAs documented patient follow-up required, specifically 44% for hospital follow-up. 54% of TTAs documented no follow-up. In summary, 88% of EDSs documented follow-up in comparison to 46% of TTAs. These findings may be a limitation of the study i.e. patient selection rather than failings in documentation.
Instructions for GP and functional status.
Coincidently, 92% of TTAs did not document ‘instructions for GP’ in contrast to 92% of EDSs that did. ‘Instructions for GP’ is not a criterion on the TTA document.
Functional status.
‘Functional status’ is also not a criterion on the TTA document and so all TTAs were not complete for this. 64% of EDS had a completion rate for documenting ‘functional status’. Functional status indicates a patient’s mobility status, self-care abilities, hearing and sight impairment.
Discussion:
This audit has established that the EDS has a higher completion rate for criteria on the discharge summary, significantly so for documenting diagnosis, co-morbidities, investigations, drug history and instructions for the GP.
One major concern that has been highlighted in performing this audit is the documentation of co-morbidities. Due to variations in training many doctors are unaware of how and where to enter this information on the EDS – there is a specific window that opens on the software program to input this information. Junior doctors were documenting patients’ past medical history under the field of ‘diagnosis’. Co-morbidities should not be listed under ‘diagnosis’ - this infers a new diagnosis - as they are not the acute problem.
The coding of the diagnosis [the acute problem], in context of a patients co-morbidities, results in a condition specific ‘fee’ being paid to secondary care. For example the ‘fee’ received for a patient diagnosed with a respiratory tract infection is different for that when the patient is diagnosed with a respiratory tract infection on the background of dementia. Inaccuracies in diagnosis lead to incorrect coding and measures of incidence. Co-morbidity is ‘any condition which co-exists in conjunction with another disease’. It is a requirement of the discharge summary to document certain co-morbidities – as determined by the Clinical Coding Co-morbidity Working Group (CCCWG)5. Although the discharge summary is not the recommended source documents for use in clinical coding – patients medical notes are used instead – it can help direct and inform those responsible for clinical coding. In should be borne in mind that it is the treating clinicians’ responsibility to document co-morbidities relevant to the current admission. Accurate and correct clinical coding will result in financial gains. Clinical coding has more important purposes other than just financial; it allows the monitoring of health services, epidemiological research, NHS planning of provisions, as well as clinical audit and governance6.
The amount of information documented is user dependent; the level and amount of detail written is subjective. For example there is no guarantee that all the investigations that a patient had are documented. One doctor may provide a whole paragraph to summaries [‘review of case’] whereas another may just write one sentence. Educating those whose task it is to complete the discharge summary about how vital and important it is, along with the role it serves in healthcare management, may influence the effort and time dedicated to producing an EDS. The principles of clear, complete and concise documentation should be applied to both the patients’ discharge summary and their medical notes.
Other healthcare professionals should also contribute to producing the discharge summary, in particular occupational therapists and physiotherapists who are more aware of a patients ‘functional status’ than the doctors. More accurate completion of this item could be achieved with their input.
At the moment with the EDS software system used at BHR University Hospital Trust once an EDS has been printed there is no means of changing any of the information. It cannot be re-accessed to document new or change existing details. Often an EDS will be finalized and so printed for a patient to be discharged home on that day for the discharge then to be delayed. The discharge date document on the EDS should be the actual date the patient is discharged from hospital. Therefore it should be possible to be able to re-access and change details on the EDS.
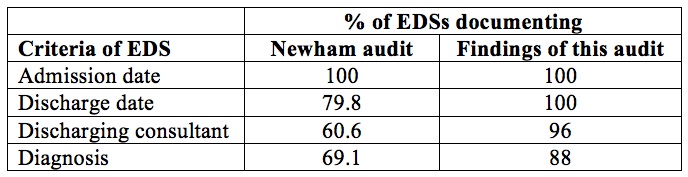
The results of this audit show that the EDS system used at BHR University Hospital Trust is better then the EDS system audited at Newham in 2008. The Newham audit did not focus on all the criteria fields of the discharge summary or compare with a hand-written discharge summary method, however there is place for comparison with the results of this audit.
Table 4: Comparison of results with findings of Newham audit
This audit has established that the EDS method provides a discharge summary more compliant with the Royal College of Physician’s recommendations on the structure and content of discharge summary in comparison to the TTA.
The EDS will inevitably replace the TTA in time. However it should be remembered that there is still a place for the TTA in clinical practice e.g. locums do not have passwords to access the software programme, if computers are not working, fail or are unavailable. At the end of the day, a discharge summary is better than no discharge summary.
Conclusion:
The findings of this audit show that the EDS is a far superior method of producing a discharge summary than the TTA. The EDS provides a more informative and detailed discharge summary, which is always legible. The discharge summary is often the only source of information a GP is given in regards to a hospital admission and therefore secondary care providers have an obligation to provide clear, complete and concise information.
This audit does highlight that there are areas for improvement and recommendation:
- The importance of a discharge summary should be highlighted to all individuals whose responsibility it is to complete them. This could promote better compliance at completing all items and completing them more thoroughly.
- EDS training should make users aware of the ‘co-morbidity’ section. Past medical history should not be listed under new diagnosis. This should be a compulsory part that has to be completed before an EDS can be finished.
- Occupational therapists and physiotherapists should be able to complete the ‘functional status’ criterion. This should be expanded to give more information and details to primary care providers.
- The documentation of certain co-morbidities (those determined by the CCCWG) should be done by ‘tick list’ selection therefore it will not rely upon the individual doctor to remember to document such co-morbidities. All the co-morbidities that should be documented could be listed and the user selects those that the patient has. This will improve the trusts performance in regards to the financial rewards linked to discharge summaries.
- The audit should be performed again in 12 months to access if EDS are maintaining high completion rates, to identify further improvement in completion rates and identify any further areas for improvement or recommendation.
- Discussion of both TTA and EDS could be a part of the regular weekly supervision of junior medical staff by their prospective consultants.
- A discharge summary should also be checked by nursing or clerical staff prior to letting the patient leave the ward to see if all components are completed.
|
Competing Interests None Declared Author Details CLAIRE POCKLINGTON, FY1, Queen’s Hospital, Romford. LOAY AL-DHAHIR, Consultant Stroke and General Medical Physician, Queen’s Hospital, Romford CORRESPONDENCE: CLAIRE POCKINGTON, FY1, Queen’s Hospital, Romford, Email: cpocklington@doctors.org.uk |
References
- GMC (2006). Good Medical Practice. London: GMC. 8, para 3.
- Royal College of Physicians (2008). A clinician’s guide to record standards – Part 1: why standardise the structure and content of medical records? London: Royal College of Physicians. 3-11.
- Kazmi, S. M. B. (2008). Quality of Electronic Discharge Summaries at Newham University Hospital: An Audit. London: British Journal of Medical Practitioners. 2008: 1(1) 30-32.
- Royal College of Physicians (2008). A clinician’s guide to record standards – Part 2: Standards for the structure and content of medical records and communications when patients are admitted to hospital. London: Royal College of Physicians. 3-11.
- NHS Classifications Service (NCS) (March 2010). Coding Clinic. London. 6:6
- Royal College of Physicians (2007). Top ten tips for coding – a guide for clinical staff. Health Informatics Unit. Royal College of Physicians.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




